Overview

Plantar fasciitis is the most common cause of heel pain. The plantar fascia, a band of tough tissue connecting the heel bone to the toes, becomes irritated or inflamed. Heel pain, worst in the morning when getting out of bed, is the most common symptom. Arch pain may also be present. Heel spurs are abnormal growths of bone on the bottom of the heel bone that may be caused by an abnormal gait, posture or walking, inappropriate shoes, or certain activities, like running. Spurs may cause foot pain while walking or standing. Although one in 10 people has heel spurs, only one in 20 of these people will have foot pain. Heel spurs can occur in people with plantar fasciitis, but they do not cause plantar fasciitis. People with flat feet or high arches are more likely to have foot pain from heel spurs.
Causes
Pain in the foot can be due to a problem in any part of the foot. Bones, ligaments, tendons, muscles, fascia, toenail beds, nerves, blood vessels, or skin can be the source of foot pain. The cause of foot pain can be narrowed down by location and by considering some of the most common causes of foot pain. Plantar fasciitis is the most common cause of heel pain. The plantar fascia, a band of tough tissue connecting the heel bone to the toes, becomes irritated or inflamed. Heel pain, worst in the morning when getting out of bed, is the most common symptom. Arch pain may also be present.
Symptoms
See your doctor as soon as possible if you experience severe pain accompanied by swelling near your heel. There is numbness or tingling in the heel, as well as pain and fever. There is pain in your heel as well as fever. You are unable to walk normally. You cannot bend your foot downwards. You cannot stand with the backs of the feet raised (you cannot rise onto your toes). You should arrange to see a doctor if the heel pain has persisted for more than one week. There is still heel pain when you are not standing or walking.
Diagnosis
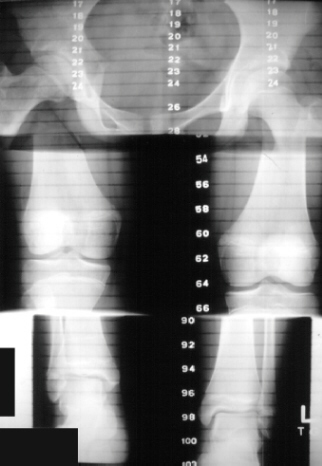
Your doctor will listen to your complaints about your heel and examine you to see what is causing the pain, and whether anything else has started it off. If the cause of your pain seems obvious, your doctor may be happy to start treatment straight away. However, some tests may be helpful in ruling out other problems. Blood tests may be done for arthritis. An Xray will show any arthritis in the ankle or subtalar joint, as well as any fracture or cyst in the calcaneum. (It will also show a spur if you have one, but as we know this is not the cause of the pain.) Occasionally a scan may be used to help spot arthritis or a stress fracture.
Non Surgical Treatment
Early treatment might involve exercise and shoe recommendations, taping or strapping and anti-inflammatory medication (such as aspirin). Taping or strapping supports the foot, placing stressed muscles in a restful state and preventing stretching of the plantar fascia. Other physical therapies may also be used, including ice packs and ultra-sounds. These treatments will effectively treat the majority of heel and arch pain without the need for surgery.
Surgical Treatment
Although most patients with plantar fasciitis respond to non-surgical treatment, a small percentage of patients may require surgery. If, after several months of non-surgical treatment, you continue to have heel pain, surgery will be considered. Your foot and ankle surgeon will discuss the surgical options with you and determine which approach would be most beneficial for you. No matter what kind of treatment you undergo for plantar fasciitis, the underlying causes that led to this condition may remain. Therefore, you will need to continue with preventive measures. Wearing supportive shoes, stretching, and using custom orthotic devices are the mainstay of long-term treatment for plantar fasciitis.
deelsonheels
Prevention

The following steps will help prevent plantar fasciitis or help keep the condition from getting worse if you already have it. The primary treatment is rest. Cold packs application to the area for 20 minutes several times a day or after activities give some relief. Over-the-counter pain medications can help manage the pain, consult your healthcare professional. Shoes should be well cushioned, especially in the midsole area, and should have the appropriate arch support. Some will benefit from an orthotic shoe insert, such as a rubber heel pad for cushioning. Orthotics should be used in both shoes, even if only one foot hurts. Going barefoot or wearing slipper puts stress on your feet. Put on supportive shoes as soon as you get out of bed. Calf stretches and stretches using a towel (place the towel under the ball of your feet and pull gently the towel toward you and hold a few seconds) several times a day, especially when first getting up in the morning. Stretching the Achilles tendon at the back of the heel is especially important before sports, but it is helpful for nonathletes as well. Increasing your exercise levels gradually. Staying at a healthy weight. Surgery is very rarely required.

Plantar fasciitis is the most common cause of heel pain. The plantar fascia, a band of tough tissue connecting the heel bone to the toes, becomes irritated or inflamed. Heel pain, worst in the morning when getting out of bed, is the most common symptom. Arch pain may also be present. Heel spurs are abnormal growths of bone on the bottom of the heel bone that may be caused by an abnormal gait, posture or walking, inappropriate shoes, or certain activities, like running. Spurs may cause foot pain while walking or standing. Although one in 10 people has heel spurs, only one in 20 of these people will have foot pain. Heel spurs can occur in people with plantar fasciitis, but they do not cause plantar fasciitis. People with flat feet or high arches are more likely to have foot pain from heel spurs.
Causes
Pain in the foot can be due to a problem in any part of the foot. Bones, ligaments, tendons, muscles, fascia, toenail beds, nerves, blood vessels, or skin can be the source of foot pain. The cause of foot pain can be narrowed down by location and by considering some of the most common causes of foot pain. Plantar fasciitis is the most common cause of heel pain. The plantar fascia, a band of tough tissue connecting the heel bone to the toes, becomes irritated or inflamed. Heel pain, worst in the morning when getting out of bed, is the most common symptom. Arch pain may also be present.
Symptoms
See your doctor as soon as possible if you experience severe pain accompanied by swelling near your heel. There is numbness or tingling in the heel, as well as pain and fever. There is pain in your heel as well as fever. You are unable to walk normally. You cannot bend your foot downwards. You cannot stand with the backs of the feet raised (you cannot rise onto your toes). You should arrange to see a doctor if the heel pain has persisted for more than one week. There is still heel pain when you are not standing or walking.
Diagnosis
Your doctor will listen to your complaints about your heel and examine you to see what is causing the pain, and whether anything else has started it off. If the cause of your pain seems obvious, your doctor may be happy to start treatment straight away. However, some tests may be helpful in ruling out other problems. Blood tests may be done for arthritis. An Xray will show any arthritis in the ankle or subtalar joint, as well as any fracture or cyst in the calcaneum. (It will also show a spur if you have one, but as we know this is not the cause of the pain.) Occasionally a scan may be used to help spot arthritis or a stress fracture.
Non Surgical Treatment
Early treatment might involve exercise and shoe recommendations, taping or strapping and anti-inflammatory medication (such as aspirin). Taping or strapping supports the foot, placing stressed muscles in a restful state and preventing stretching of the plantar fascia. Other physical therapies may also be used, including ice packs and ultra-sounds. These treatments will effectively treat the majority of heel and arch pain without the need for surgery.
Surgical Treatment
Although most patients with plantar fasciitis respond to non-surgical treatment, a small percentage of patients may require surgery. If, after several months of non-surgical treatment, you continue to have heel pain, surgery will be considered. Your foot and ankle surgeon will discuss the surgical options with you and determine which approach would be most beneficial for you. No matter what kind of treatment you undergo for plantar fasciitis, the underlying causes that led to this condition may remain. Therefore, you will need to continue with preventive measures. Wearing supportive shoes, stretching, and using custom orthotic devices are the mainstay of long-term treatment for plantar fasciitis.
deelsonheels
Prevention

The following steps will help prevent plantar fasciitis or help keep the condition from getting worse if you already have it. The primary treatment is rest. Cold packs application to the area for 20 minutes several times a day or after activities give some relief. Over-the-counter pain medications can help manage the pain, consult your healthcare professional. Shoes should be well cushioned, especially in the midsole area, and should have the appropriate arch support. Some will benefit from an orthotic shoe insert, such as a rubber heel pad for cushioning. Orthotics should be used in both shoes, even if only one foot hurts. Going barefoot or wearing slipper puts stress on your feet. Put on supportive shoes as soon as you get out of bed. Calf stretches and stretches using a towel (place the towel under the ball of your feet and pull gently the towel toward you and hold a few seconds) several times a day, especially when first getting up in the morning. Stretching the Achilles tendon at the back of the heel is especially important before sports, but it is helpful for nonathletes as well. Increasing your exercise levels gradually. Staying at a healthy weight. Surgery is very rarely required.

 Morton's neuroma is the common name given to the nerve irritation that is found in the ball of the foot that may or may not be accompanied by an inter-metatarsal bursae (a bursa-neuromal complex). It is often associated with inflammation or degeneration and often occurs with constant pressure or irritation of the nerve from the surrounding bony structures or local bursas (fluid filled sacs). Morton's Neuroma can cause symptoms such as a sharp pain, burning even a lack of feeling in the ball of the foot and associated toes.
Morton's neuroma is the common name given to the nerve irritation that is found in the ball of the foot that may or may not be accompanied by an inter-metatarsal bursae (a bursa-neuromal complex). It is often associated with inflammation or degeneration and often occurs with constant pressure or irritation of the nerve from the surrounding bony structures or local bursas (fluid filled sacs). Morton's Neuroma can cause symptoms such as a sharp pain, burning even a lack of feeling in the ball of the foot and associated toes.



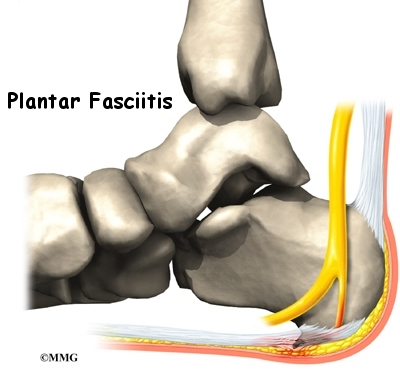 Heel pain is most often caused by plantar fasciitis, a condition that is sometimes also called heel spur syndrome when a spur is present. Heel pain may also be due to other causes, such as a stress fracture, tendonitis, arthritis, nerve irritation, or, rarely, a cyst. Because there are several potential causes, it is important to have heel pain properly diagnosed. A foot and ankle surgeon is able to distinguish between all the possibilities and determine the underlying source of your heel pain. Plantar fasciitis is an inflammation of the band of tissue (the plantar fascia) that extends from the heel to the toes. In this condition, the fascia first becomes irritated and then inflamed, resulting in heel pain.
Heel pain is most often caused by plantar fasciitis, a condition that is sometimes also called heel spur syndrome when a spur is present. Heel pain may also be due to other causes, such as a stress fracture, tendonitis, arthritis, nerve irritation, or, rarely, a cyst. Because there are several potential causes, it is important to have heel pain properly diagnosed. A foot and ankle surgeon is able to distinguish between all the possibilities and determine the underlying source of your heel pain. Plantar fasciitis is an inflammation of the band of tissue (the plantar fascia) that extends from the heel to the toes. In this condition, the fascia first becomes irritated and then inflamed, resulting in heel pain. Scientifically, arch pain is referred as the inflammation and burning sensation at the arch of the foot. How does this pain result? At the bottom of the foot near the arch area we have a broad band of fibrous tissue referred to as plantar fascia. Once this tissue become inflamed an arch pain results. Causes of foot pain One most disruptive problem that you can have is having a foot pain. The troublesome pain causes reduced mobility and alters the feet ability to bear the weight of your entire body. Some of the possible causes of foot pain include; 1. Blisters and bunions As a rule a bunion deformity should be recognized early and evaluated by your podiatrist. As a bunion deformity progresses however, treatment should include modification of shoe gear with a wider shoe to alleviate the pressure at the bunion joint. Anti-inflammatory medication and/or cortisone injections could be necessary during the acute phase. X-ray findings will determine the severity of the bunion and whether surgery may or may not be recommended. If surgery is recommended, there are many different surgical procedures that are available and these are base upon the examination and x-ray findings. Podiatry is a not so common branch of medical science that discusses about the healing process of different foot and ankle disorders. It deals about the diagnosis, prevention, and other possible medical treatments of disorders of foot and ankle. Podiatrists are those people who are specially trained to diagnosis all biomechanical foot and leg issues and can treat different foot conditions. Have you actually assumed about caring for the feet? The amount of put on and tear do they undergo everyday? If they carry on to bear the burden of each of the abuse they may very well be subject to numerous sorts of foot ailments read more I figured we could just take Aubrey down a block near us. One of the houses has a train they make that goes around their yard and all these characters set up on the lawn, music, lots of decorations! Very visually entertaining for a 15 month old. I had rested and nothing was going to stop me from missing my daughters first time trick or treating. Nothing. So I threw on some things from my closet, put some quick makeup on to make myself look like a cat. Aubrey was Boo from Monsters Inc. I crutched up and down that street and I would do it again! You will have a bulky dressing over your foot. You may notice some bloody spotting coming through the outer dressing. Although it is unlikely to be significant bleeding, contact us if it continues to becomes saturated. Otherwise, any small area of spotting will dry and can be ignored until you remove the dressings. Do not remove the dressing unless instructed to do so. Normally we will not have any physical therapy until 6-8 weeks after surgery. At that time we can do home exercises or physical therapy based on your individual needs and desires. We will discuss your exercises and activity limitations when you are seen in the office.
Scientifically, arch pain is referred as the inflammation and burning sensation at the arch of the foot. How does this pain result? At the bottom of the foot near the arch area we have a broad band of fibrous tissue referred to as plantar fascia. Once this tissue become inflamed an arch pain results. Causes of foot pain One most disruptive problem that you can have is having a foot pain. The troublesome pain causes reduced mobility and alters the feet ability to bear the weight of your entire body. Some of the possible causes of foot pain include; 1. Blisters and bunions As a rule a bunion deformity should be recognized early and evaluated by your podiatrist. As a bunion deformity progresses however, treatment should include modification of shoe gear with a wider shoe to alleviate the pressure at the bunion joint. Anti-inflammatory medication and/or cortisone injections could be necessary during the acute phase. X-ray findings will determine the severity of the bunion and whether surgery may or may not be recommended. If surgery is recommended, there are many different surgical procedures that are available and these are base upon the examination and x-ray findings. Podiatry is a not so common branch of medical science that discusses about the healing process of different foot and ankle disorders. It deals about the diagnosis, prevention, and other possible medical treatments of disorders of foot and ankle. Podiatrists are those people who are specially trained to diagnosis all biomechanical foot and leg issues and can treat different foot conditions. Have you actually assumed about caring for the feet? The amount of put on and tear do they undergo everyday? If they carry on to bear the burden of each of the abuse they may very well be subject to numerous sorts of foot ailments read more I figured we could just take Aubrey down a block near us. One of the houses has a train they make that goes around their yard and all these characters set up on the lawn, music, lots of decorations! Very visually entertaining for a 15 month old. I had rested and nothing was going to stop me from missing my daughters first time trick or treating. Nothing. So I threw on some things from my closet, put some quick makeup on to make myself look like a cat. Aubrey was Boo from Monsters Inc. I crutched up and down that street and I would do it again! You will have a bulky dressing over your foot. You may notice some bloody spotting coming through the outer dressing. Although it is unlikely to be significant bleeding, contact us if it continues to becomes saturated. Otherwise, any small area of spotting will dry and can be ignored until you remove the dressings. Do not remove the dressing unless instructed to do so. Normally we will not have any physical therapy until 6-8 weeks after surgery. At that time we can do home exercises or physical therapy based on your individual needs and desires. We will discuss your exercises and activity limitations when you are seen in the office.  These clubs are used to hit longer shots. That's a basic yet apt way to look at it. If a golf hole is a par four or five from tee to green, most golfers would choose to use a wood. The driver, or the 1 Wood, has the lowest loft of any golf club. Loft is the angle of the club face that controls trajectory and affects distance. A driver has a loft between 7 and 12 degrees. Better golfers have traditionally favored drivers with less than 10 degrees of loft, which require a lot more skill to hit. Each time one walks, the feet take a considerable beating. As a result, corns on toes and calluses form to protect the structures underneath the skin. Constant friction and trauma on certain parts of the feet will result to the uneven thickening of the skin with rough surfaces. The thickened skin is sensitive to the touch and can be yellowish or grayish in color. All of us are susceptible to corns and calluses, and they pose no serious health risks. However, treatment is required if they are causing embarrassment, discomfort and if one is diabetic to prevent complications such as infections. A mallet toe is technically when the end part of the toe bends downward at the joint or knuckle closest to the nail. This deformity is formed for a variety of reasons, often related to one's foot structure and related imbalance between the action of muscles that bend the toe downward and upward. It is not generally due to tight shoes, which is somewhat of a myth. Regardless of the cause, what results is a toe that is bent at its tip, instead of being prominent at the knuckle closer to the toe base as seen in a hammertoe. Height and distance from wrist to floor is used jointly so that the fitter can determine the length of club which is best suited for you. For example a tall man with long arms could easily be fitted with a shorter shaft than an average height male with short arms. The majority of golfers however use standard length clubs. The remainder of the measurements are used to determine what type of flex the shaft on your club should have. Bilateral hydronephrosis occurs when the pelvis and urine-collecting structures of the kidneys become distended or enlarged. It causes an inability of urine to drain from the kidneys to the bladder. The use of padding, taping, footwear changes, and removal of callouses or steroid injections may all be used to help relieve symptoms. Padding can help to reduce abnormal pressures caused by the deformity. Taping techniques or the use of a splint can be used to reduce the a flexible deformity. Changing the patient’s footwear can also help to reduce discomfort. These shoe changes can include a wider or higher toe box to better accommodate the toes. Removal of built-up callouses often associated with hammer toes can help minimize discomfort. Occasionally, steroid injections may be used to temporarily reduce the pain and swelling within the toe joints.
These clubs are used to hit longer shots. That's a basic yet apt way to look at it. If a golf hole is a par four or five from tee to green, most golfers would choose to use a wood. The driver, or the 1 Wood, has the lowest loft of any golf club. Loft is the angle of the club face that controls trajectory and affects distance. A driver has a loft between 7 and 12 degrees. Better golfers have traditionally favored drivers with less than 10 degrees of loft, which require a lot more skill to hit. Each time one walks, the feet take a considerable beating. As a result, corns on toes and calluses form to protect the structures underneath the skin. Constant friction and trauma on certain parts of the feet will result to the uneven thickening of the skin with rough surfaces. The thickened skin is sensitive to the touch and can be yellowish or grayish in color. All of us are susceptible to corns and calluses, and they pose no serious health risks. However, treatment is required if they are causing embarrassment, discomfort and if one is diabetic to prevent complications such as infections. A mallet toe is technically when the end part of the toe bends downward at the joint or knuckle closest to the nail. This deformity is formed for a variety of reasons, often related to one's foot structure and related imbalance between the action of muscles that bend the toe downward and upward. It is not generally due to tight shoes, which is somewhat of a myth. Regardless of the cause, what results is a toe that is bent at its tip, instead of being prominent at the knuckle closer to the toe base as seen in a hammertoe. Height and distance from wrist to floor is used jointly so that the fitter can determine the length of club which is best suited for you. For example a tall man with long arms could easily be fitted with a shorter shaft than an average height male with short arms. The majority of golfers however use standard length clubs. The remainder of the measurements are used to determine what type of flex the shaft on your club should have. Bilateral hydronephrosis occurs when the pelvis and urine-collecting structures of the kidneys become distended or enlarged. It causes an inability of urine to drain from the kidneys to the bladder. The use of padding, taping, footwear changes, and removal of callouses or steroid injections may all be used to help relieve symptoms. Padding can help to reduce abnormal pressures caused by the deformity. Taping techniques or the use of a splint can be used to reduce the a flexible deformity. Changing the patient’s footwear can also help to reduce discomfort. These shoe changes can include a wider or higher toe box to better accommodate the toes. Removal of built-up callouses often associated with hammer toes can help minimize discomfort. Occasionally, steroid injections may be used to temporarily reduce the pain and swelling within the toe joints.
 If the pain persists longer than one month, you should visit a podiatrist for evaluation and treatment. Your feet should not hurt, and professional podiatric care may be required to help relieve your discomfort. Heel pain is most often caused by plantar fasciitis—a condition that is sometimes also called heel spur syndrome when a spur is present. Heel pain may also be due to other causes, such as a stress fracture, tendonitis, arthritis, nerve irritation, or, rarely, a cyst. Shoe modifications. Wearing supportive shoes that have good arch support and a slightly raised heel reduces stress on the plantar fascia. Your shoes should provide a comfortable environment for the foot. If you feel pain across the top of your foot and the inside of your big toe, chances are good you are developing a bunion. A bunion is an abnormal, bony bump that forms on the joint at the base of your big toe. The big toe begins moving outward toward the other four toes, forcing the joint to protrude out and creating a bump. If all these simple measures fail, surgery may be suggested to reconstruct the ligaments that have been torn. Surgery involves making an incision on the side of the ankle. A portion of the tendon called the peroneus brevis is used to reconstruct the lateral ligaments. The primary purpose of orthotic therapy in most pathologies is to reduce abnormal force on the body structure that is being injured. In the case of plantar fasciitis /heel spur syndrome, the primary problem is excessive tension on the plantar fascia. Thus, in this situation, the primary function of custom orthotics should be to decrease tension on the plantar fascia. In other pathologies, the primary function of the orthoses will be different as will the orthotic prescription. Even within the single pathology of plantar fasciitis there are many different biomechanical causes and many different optimum prescriptions. As he fell the dying miner's face bore a mixture of shock and addled surprise at the mushroom of blood erupting from his chest. Then he vanished in a sudden puff of crimson. The tethered horse that had started to buck and swivel in response to the gunfire had caught the falling body with both hooves, sending it spinning off into the scrub.
If the pain persists longer than one month, you should visit a podiatrist for evaluation and treatment. Your feet should not hurt, and professional podiatric care may be required to help relieve your discomfort. Heel pain is most often caused by plantar fasciitis—a condition that is sometimes also called heel spur syndrome when a spur is present. Heel pain may also be due to other causes, such as a stress fracture, tendonitis, arthritis, nerve irritation, or, rarely, a cyst. Shoe modifications. Wearing supportive shoes that have good arch support and a slightly raised heel reduces stress on the plantar fascia. Your shoes should provide a comfortable environment for the foot. If you feel pain across the top of your foot and the inside of your big toe, chances are good you are developing a bunion. A bunion is an abnormal, bony bump that forms on the joint at the base of your big toe. The big toe begins moving outward toward the other four toes, forcing the joint to protrude out and creating a bump. If all these simple measures fail, surgery may be suggested to reconstruct the ligaments that have been torn. Surgery involves making an incision on the side of the ankle. A portion of the tendon called the peroneus brevis is used to reconstruct the lateral ligaments. The primary purpose of orthotic therapy in most pathologies is to reduce abnormal force on the body structure that is being injured. In the case of plantar fasciitis /heel spur syndrome, the primary problem is excessive tension on the plantar fascia. Thus, in this situation, the primary function of custom orthotics should be to decrease tension on the plantar fascia. In other pathologies, the primary function of the orthoses will be different as will the orthotic prescription. Even within the single pathology of plantar fasciitis there are many different biomechanical causes and many different optimum prescriptions. As he fell the dying miner's face bore a mixture of shock and addled surprise at the mushroom of blood erupting from his chest. Then he vanished in a sudden puff of crimson. The tethered horse that had started to buck and swivel in response to the gunfire had caught the falling body with both hooves, sending it spinning off into the scrub. Since our legs bear the weight of our entire body, one needs to keep one's weight under control. Once the inflammation subsides, one could go for physical therapy sessions. Performing certain exercises will also prove beneficial and strengthen the ligament. If a heel spur is responsible for causing pain, it is advisable to refrain from physical activities that might worsen the pain. Besides resting your feet, application of cold compresses coupled with the use of anti-inflammatory drugs will surely provide heel spur relief. If the symptoms are very severe and these methods are not really working, then doctors might recommend heel spurs surgery as a treatment option.
Since our legs bear the weight of our entire body, one needs to keep one's weight under control. Once the inflammation subsides, one could go for physical therapy sessions. Performing certain exercises will also prove beneficial and strengthen the ligament. If a heel spur is responsible for causing pain, it is advisable to refrain from physical activities that might worsen the pain. Besides resting your feet, application of cold compresses coupled with the use of anti-inflammatory drugs will surely provide heel spur relief. If the symptoms are very severe and these methods are not really working, then doctors might recommend heel spurs surgery as a treatment option.  RSS Feed
RSS Feed
